

Arundi Venkayyya
Curator of EngagingPatients.org
A common mantra in pediatric healthcare is that children are not tiny adults. The distinction between children and adult medical care is particularly evident when it comes to EHR issues. Although a significant number of pediatric practitioners use EHRs, these electronic records lack functionality designated for pediatrics in particular, and these gaps can lead to serious medical risks for young patients.
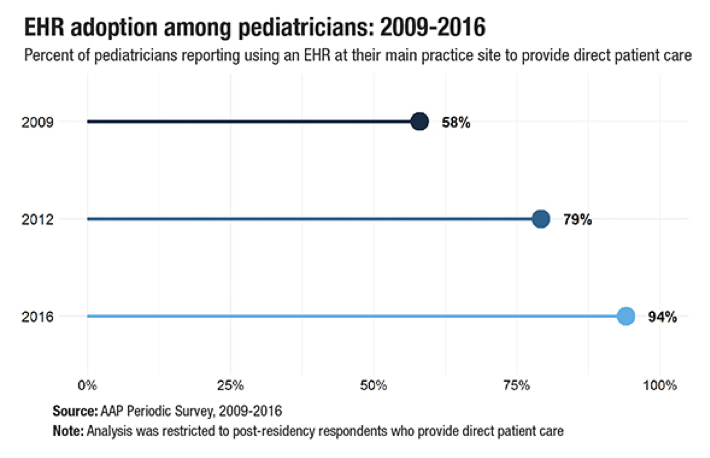
According to a 2018 American Academy of Pediatrics survey, 94 percent of pediatricians reported using EHRs at their main practice sites in 2016. That number was a significant increase over the 79 percent who reported using them in 2012. Despite this growth, few pediatricians report using “fully-functional, pediatric-specific EHRs that include features such as weight-based dosing, tracking immunization schedules and plotting growth charts (8 percent in 2012 and 17 percent in 2016).”
Which leads us back to the point that children are not little adults. There can be serious medical implications if an EHR doesn’t consider pediatric-specific standards.
There aren’t any existing standards for the integration of pediatrics into EHRs. However, the 21st Century Cures Act encourages the Office of the National Coordinator for Health Information Technology to incorporate voluntary rules for EHR usage for pediatrics.
To help inform policymaking around the 21st Century Cures Act, a team from the Pew Charitable Trusts worked with clinicians at two children’s hospitals to “identify and investigate incidents in which EHRs reportedly contributed to drug prescribing or administration errors that jeopardized safety for pediatric patients.”
In a new issue brief, the Pew team reported that by examining error reports, researchers at each facility found thousands of these cases. Their brief describes 12 cases that demonstrate functional issues with EHRs in pediatric settings that could lead to unsafe conditions for children receiving care.
The 12 cases are divided into four broad categories of EHR issues that jeopardize children’s health:
- Information display: information is displayed in confusing ways; data are missing or hard to find
- Difficult data entry: entering data is challenging, leading to delays or workarounds
- Feedback: EHRs don’t indicate that an action has been taken such as when a patient has received a medication
- Workflow: care coordination across team members or other departments or facilities is challenging
Examples of issues include:
Information display:
Some EHRs only allow measurement in U.S. customary units (pounds and inches) instead of the metric units traditionally used in medicine. In one case, a clinician entered a child’s weight in pounds when the EHR was configured to receive weight in kilograms. The misunderstanding effectively doubled the child’s actual weight, resulting in the patient later receiving twice the appropriate acetaminophen dose. Given the potential for errors, EHRs should clearly specify appropriate units of measurement and flag when potentially erroneous values have been entered. Without safeguards, staff can unknowingly submit wrong data that lead to treatment errors.
Difficult data entry:
EHRs can have built-in processes such as standard vaccination schedules based on date of birth. These features are intended to reduce data entry but can create risks if clinicians can’t override them when appropriate. In one case, a four-month-old infant was admitted to the hospital. The EHR’s default settings automatically checked a box to indicate that the infant was older than six months old and generated a vaccination schedule based on the incorrect information. Clinicians spotted the EHR’s mistake and didn’t give the inappropriate vaccines, but the system wouldn’t let them uncheck the box listing the wrong age or modify the vaccine plan. These types of errors could lead to harm; physicians and nurses treating the patient in the future could rely on incorrect information when making decisions, and other clinicians might not have identified the mistake to begin with.
Feedback:
EHRs can offer preset choices for the length of a prescription such as five, 10, or 30 days to help calculate how much of a drug should be dispensed. However, in one case, a provider intended to prescribe indefinite antiviral therapy for a transplant patient but accidentally selected the EHR’s preset 30-day, “no refills” prescription order. The error was identified at a follow-up visit after a five-day treatment lapse that increased the risk of infection and transplant rejection.
Workflow:
Clinicians use EHRs to document many facets of care, but some systems don’t have the necessary features to treat patients with complex medical needs. In these cases, clinicians might document care in both the EHR and by other means, including on paper — a fragmented documentation approach that can lead to harm. In one hospital, oncologists use a combination of the EHR and a paper chart to manage patients’ chemotherapy. When a patient received a scheduled dose of vincristine, a powerful cancer medication, the treatment was documented in the EHR but not on the paper chart. When reviewing the paper chart, clinicians concluded that the patient had missed the scheduled treatment and administered an additional and unnecessary dose without consulting the EHR.
These alarming risks to pediatric patients might be avoided if EHR developers and clinicians work together to identify risks and gaps and complete post-implementation testing to evaluate performance. It’s critical to remember that children require different care than adults do.

