HEALTHCARE SOLUTIONS
PARTNER WITH
HEALTHCARE EXPERTS
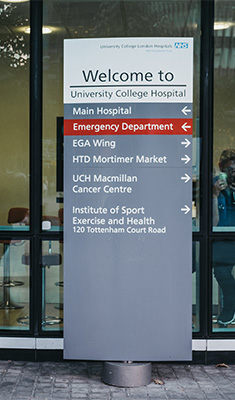
We’re passionate about healthcare and helping you share the right information at the right time with patients, families, payers, providers and staff. Learn more about how we can help you improve outcomes and boost engagement.