

Chelsea Youngquist
Director of Marketing
“Informed consent is not just the signing of a form. Informed consent is about a thorough process of communication between patient and provider,” says Aaron Fink, MD.
As care providers, ensuring that our patients understand the goals and possible outcomes of treatments remains a top priority. The process of informed consent is so much more than checking boxes on a form, and it all starts with effective communication.
There are many challenges that affect obtaining real informed consent.
1) Patient comprehension – Patients often have poor recall of information discussed during the informed consent process and their comprehension level is frequently overestimated.
2) Patient use of information – Patients do not always use information disclosed during the informed consent conversation rationally. Some may make decisions based on instinct or their feelings about the surgeon.
In addition, patients may feel pressure to sign the consent form, and many others perceive it as just another paper to sign.
3) Patient autonomy – The informed consent process assumes that patients make care decisions independently. Studies show that this isn’t always the case. Many prefer to make decisions collaboratively with their support systems, or even defer to members of that group for decision-making.
4) Demands on providers – A quality process is demanding and takes time from busy clinical schedules.
5) Providers meeting standards – Research suggests that minimal informed consent standards are rarely met. In fact, in a study of 2553 clinical decisions made during 1057 patient-physical encounters, only 9% met the criteria for completely informed decision-making.
What can providers do to improve the process?
1. Most importantly, create and support a culture of clear and open patient-provider communication, and especially involve patients in decisions.
- Improve patient comprehension by ensuring providers are using language that patients can easily understand, rather than medical jargon.
- Ideally and whenever possible, communicate in the language most comfortable for the patient.
- Focus on shared decision-making. Medical treatment is a partnership between patient and clinician. The moral responsibility for decisions is carried by both partners.
2. Ensure clinicians understand goals and standards.
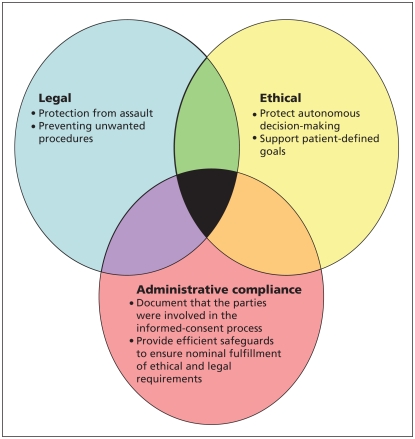
- Recognize that there are several purposes to informed consent. Allow the process sufficient flexibility to fulfill its varied purposes.
3. Utilize technology to keep communication clear and concise.
Getting paper out of the process increases convenience, helps ensure consent documents are accurate and up to date, and that forms are not lost. It can also improve patient comprehension and satisfaction.
Studies have shown that a computer-based consent tool improved patients’ comprehension of procedure-specific risks.
Another online tool improved patient satisfaction and self-rated comprehension for several procedures, and when compared with written consent forms, the online tool objectively improved patient comprehension of risk, benefits and alternatives.
Informed consent is so much more than checking the box. Creating and supporting a culture of open communication, clear expectations and shared decision-making fosters deep respect for patients, improves their satisfaction and helps to minimize any legal conflict.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3307558/



